I wanted to share this article about the effects of hydrocortisone dosing on mood and energy, “Hydrocortisone Affects Fatigue and Physical Functioning Through Metabolism of Tryptophan: A Randomized Controlled Trial” and let you know something I just realized. I feel like this is a very important post because this article proves to me that steroid dependence contributed to my 11 year old’s vitamin A toxicity.
It seems that Vitamin A metabolism is altered by multiple factors. I have clients who have multiple medical issues that are also vitamin A toxic. It has to do with different medications that they take that also impair vitamin A metabolism. These medications include Miralax, Melatonin, H2 receptor antagonist, excess vitamin C, Metformin, and Lasix (see this post). The list continues to get longer and longer. So it seems that vitamin A metabolism is easily altered by many medications, but also diet (oxalate, aldehydes, alcohol). Detoxification of retinoic acid from the body is also altered by many factors (see this post).
SUMMARY – for those who don’t like long winded explanations.
- Hydrocortisone (HC) at higher doses has a paradoxical effect on Tryptophan metabolism – This helps with mood and perceived energy
- HC at higher doses causes LESS tryptophan to become niacin
- Low niacin leads to low NAD
- Low NAD leads to low metabolism of vitamin A from retinol and retinal (beta-carotene is a source) to retinoic acid
- This means our kids are at risk for vitamin A toxicity
- Vitamin A only leaves the body as retinoic acid
- They also may appear to be vitamin A deficient due to low retinoic acid
- Insufficient HC can also lower niacin (lower NAD) as cortisol controls the enzyme action in the first stage of Tryptophan metabolism.
- Overall, kids on HC are at risk for poor vitamin A metabolism from altered NAD levels.
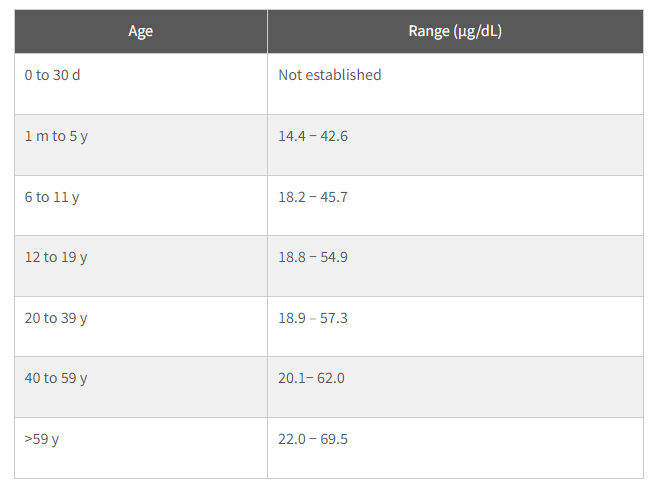
- Have serum vitamin A (retinol) checked. There is a screen shot int this post of “normal” values as some labs have ridiculously high levels set.
- Even if serum vitamin A levels are “normal” we don’t know how much is in our kiddos livers.
- If your child is iron deficient as well, this sets them up for hepatic vitamin A toxicity because iron deficiency prevents the mobilization of vitamin A from storage.
- If you are giving a niacin supplement along with HC, and your child is insanely fatigued, it could be that their tryptophan levels are WAY too high because niacin blocks the enzyme that starts the kynurenine pathway, and hydrocortisone, depending on the amount used, could also be blocking this pathway.
Signs of poor metabolism of vitamin A (or retinol/retinal toxicity, but retinoic acid deficiency)
- eczema
- histamine intolerance
- poor wound healing
- bleeding gums
- nausea
- headache
- high VLDL and/or LDL
- insulin resistance
- low platelet count (retinoic acid toxicity)
- high platelet count (possible retinol toxicity symptom)
- low TSH
- high total T4
- keratosis pilaris (chicken bump skin)
- dry cracked heels
- hair loss (male pattern baldness, losing eyebrows)
- hypercalciuria
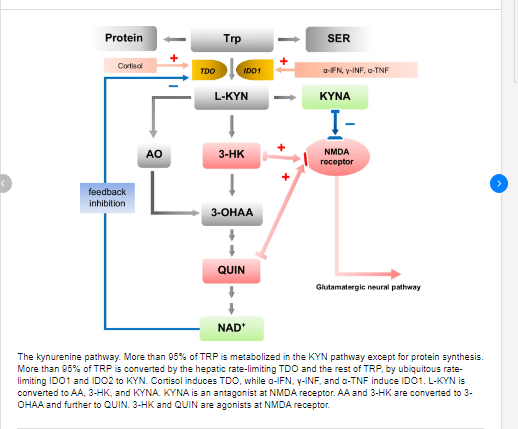
I’m a dietitian and I have been studying vitamin A toxicity and related metabolic pathways. Vitamin A Toxicity can occur in a low NAD state. NAD is a cofactor for enzymes that convert retinol and retinal (beta-carotene come in at retinal), to retinoic acid. NAD contains niacin. Niacin can be a supplement, but we make niacin from the amino acid tryptophan,. Approximately 95% of the Tryptophan in our body is pushed through this pathway to make niacin. The other 5% is typically used to make Serotonin.
That being said, my girls have late onset congenital adrenal hyperplasia. My 17 year old wasn’t diagnosed until 12 years old. She suffered miserably for years from eczema, allergies, and fatigue. She still does unless she “half” stress doses. She has been accused by her doctor of “over medicating”. She says that doing a half stress dose helps so much with everything! Her fatigue, her eczema, her allergies, but she is trying to be obedient to the doctor’s orders.
So, here is what I just figured out. Cortisol turns on the first enzyme in the pathway that pushes tryptophan to Niacin. If Cortisol is too low, then niacin may also be low. Paradoxically, when increasing hydrocortisone, niacin production from tryptophan goes even lower. Both corstisol deficient and over abundance of hydrocortisone can cause low production of NAD. NAD is needed to convert retinol to retinal and then into retinoic acid. When retinol is high, it causes a histamine reaction! ALLERGIES and HIVES! When retinoic acid is low it means skin can’t heal! CHRONIC ECZEMA. When retinoic acid is low, we can’t get Vitamin A out of the body. It only leaves in that form. VITAMIN A TOXICITY!
POSSIBLE HISTORY OF VITAMIN A TOXICITY WITH PROBABLE MAXED OUT LIVER STORES IN MY 17 YEAR OLD WITH NCCAH
My 17 year old was likely vitamin A toxic last year until she started stress dosing all the time because she felt bad. I say I think she was likely vitamin A toxic because her labs showed a low TSH and high retinol in the blood will cause a low TSH. Her TSH is now normal, but she is still feeling tired and fatigued. Her serum vitamin A is 39 (normal value <59 for her age). Last year she became allergic to chocolate and beans. She had to stop eating them. They are high oxalate foods that also can cause low NAD levels (see my blog for details www.weakthereforestrong.com/blog). When she stopped eating these foods, it helped increase her NAD recycling. However, I think she still has overall high vitamin A levels due to her histamine intolerance goes up and down. I think she, at times, mobilizes vitamin A quickly from stores and triggers a histamine release from mast cells. Her skin still looks terrible, too, and she has very thin blood. All signs of vitamin A toxicity.
DEFINITELY VITAMIN A TOXICITY IN MY 11 YEAR OLD WITH NCCAH
However, my 11 year old is vitamin A toxic. I think this Kynurenine pathways is part of the reason why. The other part is because we were accidentally feeding her high oxalate plantain flour. We thought it was low oxalate due to a dietitian handout that was wrong. Oxalate impairs the enzyme lactate dehydrogenase which makes NAD low resulting in vitamin A metabolism slowing down. You can read more about that on this blog, but I just realized that her NCCAH plays a HUGE role in this as well.
So, something else….this past January I was tired of my daughter using steroids to make herself feel better. Her diet is pretty limited because of foods allergies and so I decided to make her take a multivitamin. This contained vitamin A and niacin. She became even more tired and her eczema worsened. She is sleeping all day.
ORAL NIACIN, GOOD OR BAD FOR KIDS WITH CAH?
Well, when you add Niacin to the body in supplemental form. It inhibits the enzyme TDO. This essentially shuts of Tryptophan conversion to niacin, and remember, 95% of tryptophan in the body goes through this pathway, or it is made into serotonin. I think that what is happening to my daughter is that her serotonin levels are way too high because I blocked tryptophan metabolism into niacin.
Interestingly, though, this study I link to below showed an increase in tryptophan from using more hydrocortisone, which I feel is the opposite of what I would think. This actually worries me even more. This would mean that increasing doses of steroids may lead to even less niacin being made in the body! This means a low NAD state. There may be a paradoxical effect when doses are high versus low.
In any case, I think using oral niacin has pushed my daughter into an extremely high tryptophan state as she has also been stress doing. So, now we are avoiding niacin all together to see if this will help her to be able to push more tryptophan down this pathway and stop her from feeling so exhausted, and also stop her wanting to take mores steroids. I do think half stress dosing is probably worsening her NAD levels though, especially as this study shows that high dose steroids push everything back to tryptophan.
(Another important thing to note is that the supplement Nattokinase blocks the other enzyme IDO1. Taking both Niacin and Nattokinase will alter tryptophan metabolism completely. This may cause serotonin syndrome, especially in someone taking a SSRI)
CHECK KIDS ON HYDROCORTISONE FOR VITAMIN A TOXICITY
Also, I think that our kids should be checked for vitamin A toxicity. NAD is crucial for the metabolism of Retinol, Retinal, and Beta-carotene to retinoic acid. Excessive amounts of retinol in the body can cause histamine intolerance (retinol triggers mast cell histamine release), diabetes (high retinol binding protein 4), and bone loss (high retinol triggers osteoclasts to break down bone quickly leading to hypercalciuria).
High retinal levels can contribute to neurodegenerative disease and macular degeneration through combining with an ether lipid called ethanolamine making A2E. This A2E aggravates microglia cells and could be causing brain inflammation and is known to cause macular degeneration.
Low retinoic acid means poor wound healing, worsening eye sight, and poor growth. Retinoic acid is the only form of vitamin A that can leave the body. So if a person is low on NAD, they will become toxic in vitamin A.
Vitamin A is stored in the liver, until it reaches maximum capacity. After which the body will shuttle vitamin A packaged into cholesterol out of the liver in attempts to store it in adipose tissue. This makes blood cholesterol levels go up. So if your kiddo has high cholesterol, this is likely the cause.
When retinol is high, it can cause insulin resistance which will result in high triglycerides or at minimum a triglyceride:HDL ratio greater than 3.5 on labs which will indicate insulin resistance which will eventually become diabetes.
MONITORING NAD IS IMPORTANT
So it’s important for our kids to have normal NAD levels. This can be altered due to them being steroid dependent. Cortisol induces the production of niacin in the body. Adding a niacin supplement will inhibit this pathway and make them TIRED as heck, at risk for serotonin syndrome, but they may be better metabolizers of vitamin A, if they aren’t impairing their metabolism in other ways (high oxalate foods, melatonin, miralax, etc.) Maybe kids with CAH need to monitor things that lower cellular NAD levels.
Here is a general description of the kynurenine pathway.https://www.researchgate.net/…/The-kynurenine-pathway…
Here is a paper supporting the fact that increasing hydrocortisone decreases fatigue due to altering tryptophan levels via the kyrenurine pathway.https://academic.oup.com/jcem/article/103/9/3411/5047295
I’m a dietitian, not a doctor. This post was written only to inform, and to share, because I seriously care about how our kids feel. Please consult with a physician before making any changes to medications, diet, supplements or lifestyle.
