I am a dietitian. I am not a doctor. This is not medical advice, but only written to inform. Please consult with your personal health care practitioner before starting or stopping supplements or medications, and before making any changes to your diet.
Simple Sum Up
- Melatonin is known to help induce sleep
- It often doesn’t keep us asleep because it is metabolized away in about four hours
- High dose Melatonin (above 3 mg in children and above 5 mg in adults) is NOT good for the brain
- Melatonin catabolism uses ADH and ALDH
- ADH and ALDH are also enzymes that metabolize Vitamin A
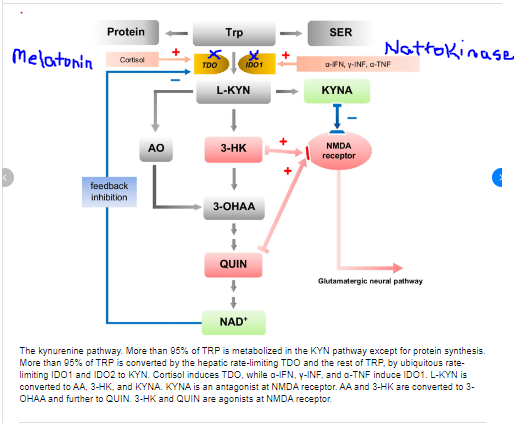
- Melatonin also inhibits TDO enzyme of the Kynurenine pathway
- This stops the production of NAD in the liver, kidneys, and brain
- NAD is a cofactor for the enzymes that metabolize vitamin A
- High dose Melatonin will cause vitamin A to stay in its retinal/retinol form.
- Excess retinal in the brain can bind to ethanolamine.
- Phosphatidyl-ethanolamine is a precursor for choline synthesis.
- Low choline levels leads to low acetylcholine which is the major neurotransmitter of the gut, brain, and heart (think slow gut, slow brain, slow heart.)
- Also, when ethanolamine combines with retinal it can form A2E which is a schiffs base. This aggravates microglia cells which causes inflammation in the brain in my opinion. (Is my child drunk and also toxic on retinaldehyde?)
This post could pertain to adults who take more than 5 mg per day or to children taking more than 3 mg per day. Also anyone who doses melatonin multiple times a day, and anyone who has been on oral melatonin for quite some time may be at risk for all discussed below. Monitor yourself for symptoms of melatonin toxicity at the body of this article.
MELATONIN FOR SLEEP?
Melatonin is often prescribed to individuals with autism and intellectual disability because these people often struggle with sleep. In fact, the MBD5 deletion mouse model of Zoey’s genetic syndrome makes less circadian rhythm proteins in general. This leads to a predisposition for, what I like to call, InZomnia. We did give Zoey melatonin on and off for a few months when she was around two years old, but she would also have worse “drunk days” after taking melatonin. She would run into walls, so we stopped this supplement. I’m actually glad we did. We did have to learn how to promote better sleep hygiene in alternative ways. I think if we had kept using melatonin, she would have worse hypervitaminosis A than she does now.
The reason why Zoey was more “drunk” the day after taking melatonin is that high dose Melatonin actually alters NAD levels in the brain and also can compete with enzymes for alcohol and aldehyde metabolism. I will explain further….
MELATONIN and the KYRURENINE PATHWAY
https://www.researchgate.net/publication/339877327_Antidepressant-like_effects_of_kynurenic_acid_in_a_modified_forced_swim_test
High dose melatonin inhibits the enzyme TDO in the liver, brain, and kidney. This lowers NAD production. I believe this is in a dose dependent manner. The more melatonin given, the more this enzyme is blocked. The more often melatonin is dosed, the lower NAD production will be in these organs. This will cause higher amounts of retinol/retinal in these organs, and low levels of retinoic acid. Low levels of retinoic acid in the brain can alter nerve conduction by altering how many voltage gated calcium channels are open.
MELATONIN NEEDS ADH and ALDH FOR CATABOLISM
In addition, to actually blocking NAD production, melatonin may competitively impair retinol/retinal metabolism. Melatonin is metabolized using the enzymes alcohol dehydrogenase and aldehyde dehydrogenase. These enzymes are also used in vitamin A metabolism. Large doses of melatonin could compete with Vitamin A for metabolism resulting in a retinoic acid deficiency. Again, alterations in retinoic acid levels could contribute to changes in nerve conduction and either slow the brain down or speed it up by altering how many voltage gated calcium channels are open.
In addition, consider that if these enzymes in the brain are metabolizing melatonin, this could lead to higher levels of endogenously produced alcohols and aldehydes in the brain and could be the cause of the “drunk symptoms” that Zoey gets the morning after melatonin.

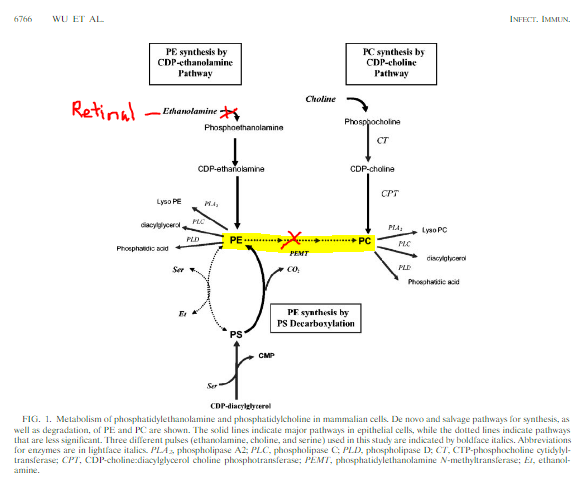
Adapted from ….https://journals.asm.org/doi/10.1128/IAI.72.12.6764-6772.2004
FURTHER CONSEQUENCES OF MELATONIN ALTERING VITAMIN A METABOLISM
The inability to convert retinol to retinoic acid in the liver leads to increased hepatic storage of retinol as retinyl esters which can lead to liver toxicity as well as a further burden on choline as it is needed for the enzyme Lecithin Retinol Acetyltransferase (LRAT) which helps to store vitamin A . (I will post soon about how low levels of retinoic acid in the kidney can cause kidney disease.)
High levels of retinal in the brain can complex with ethanolamine, an amino acid that is typically part of an important ether lipid that provides structure to the brain and helps it move smoothly. You can read more about how retinal and ethanolamine combine to form A2E, a schiffs base which aggravates microgrial cells resulting in brain inflammation and neurodegeneration here.
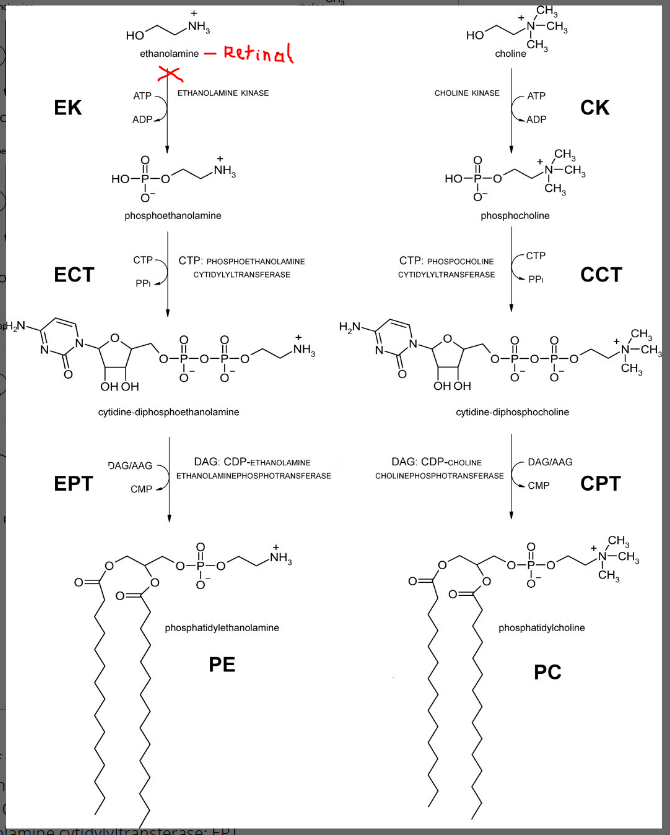
Phosphatidyl-ethanolamine is actually a precursor choline synthesis as well, so in a round about way, melatonin is actually placing a huge burden on choline needs in the liver and the brain. Melatonin keeps retinal from becoming retinoic acid by altering NAD levels and also tying up ALDH in metabolism. This leads to high levels of retinal which can bind to ethanolamine. Low levels of phosphatidyl ethanolamine makes the body more reliant on dietary choline to produce phosphatidyl choline. More choline will be sequestered into the CPD-choline pathway shown below which means less choline is available for acetylcholine production (again…think slow gut, slow brain, and slow heart.)
PROOF THAT MELATONIN ALTERS VITAMIN A METABOLISM?
I have a friend in our 2q23.1 (MBD5) deletion support group who share a recent story of starting melatonin for sleep. As she increased her daughter’s dose of melatonin, there was a dose related response in blood glucose levels. As the dose went up, blood glucose levels went up. It is quite possible that as the dose increased, NAD levels decreased to the point that retinol levels increased, and retinoic acid levels decreased. High RBP4 can actually causes insulin resistance which would cause hyperglycemia (https://pubmed.ncbi.nlm.nih.gov/16034410/), and high retinoic acid can cause hypoglycemia (https://pubmed.ncbi.nlm.nih.gov/20032483/).
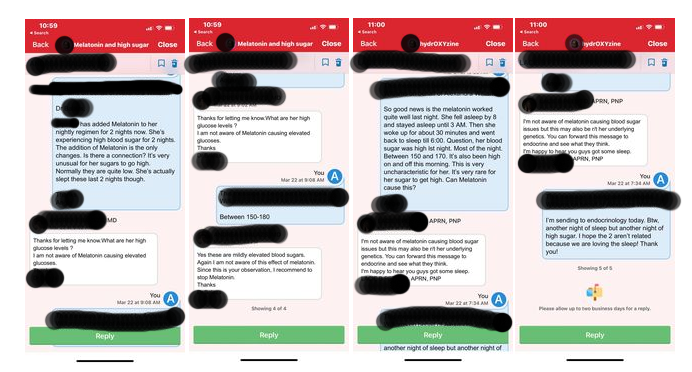
Here is our conversation….
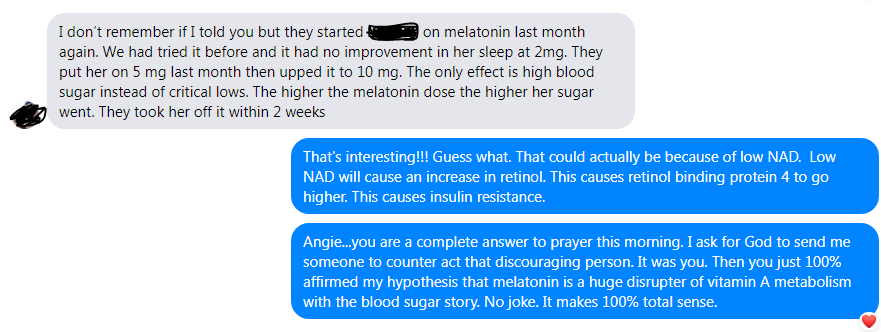
And here is the conversation she had with different care providers about the high blood glucose from Melatonin.
WHAT IF THE SIDE EFFECTS OF MELATONIN OVERDOSE ARE ACTUALLY SIGNS OF RETINOIC ACID DEFICIENCY?
Alopecia and dermatological manifestations of melatonin overdose could actually be related to retinoic acid deficiency. In addition, when metabolizing large amounts of melatonin, NAD is used which may contribute to low cellular levels of NAD. This can result in impaired energy (ATP) levels leading to the symptoms described in melatonin overdose such as fatigue. This could also cause buildup of lactate resulting in lactic acidosis which would account for the vomiting seen in melatonin overdose.

https://www.sleepfoundation.org/melatonin/melatonin-overdose
WHAT’S A BETTER SLEEP SOLUTION???
Okay….so not to pull the “my child is more disabled than your child” card here, BUT the mouse model of MBD5 deletion doesn’t make very much circadian rhythm proteins. However, we got Zoey to sleep WITHOUT melatonin! Woohoo! If we can do it and genetics is playing a huge role against us, then you can do it too! How did we do it?
Sleep Hygiene.
- Dark room
- Cold room
- Warm bath before bed
- No screens (blue light) two hours before bed
- Verilux happy light (or other light therapy light) in the morning for 30 minutes OR natural sunlight to trigger the timing of melatonin release for 12 hours later.
- Prayers before bed. <3
Overall I do NOT recommend melatonin supplementation. The end.
